The outbreak of the disease in the western world has exposed the tension between the need to provide important health-related information to everyone who needs it versus the concern of harmful stigmas
On May 7 2022, the UK Health Security Agency (UKHSA) reported a case of monkeypox in a patient who had recently returned from Nigeria. The disease itself is not new. The virus that causes it is found naturally in central and western Africa, where occasional outbreaks occur mostly when humans who are in contact with other mammals become infected. Up until the current outbreak, the only case of monkeypox in Israel was discovered in 2018, an Israeli returning from Nigeria.
Since the first report in the UK, several thousand new cases have been detected outside of Africa. They were not related to the first patient and usually not related to each other. Most patients also did not travel to countries in which the disease is naturally and routinely present. By Thursday, June 23, 3,411 monkeypox cases were identified across all continents except Antarctica, including 16 cases in Israel.
The current outbreak is garnering great interest. This is the first time that monkeypox cases are being detected across a number of continents simultaneously, including some patients who contracted the disease without having recently visited Africa, and without having a known contact with other diagnosed patients. The current outbreak is of great interest. This is also the first time that an outbreak of monkeypox is being reported among men who have sex with men (MSM) – a group that includes men who are curious and prone to experimenting as well as bisexuals and homosexuals. This is also the first time that the spread of monkeypox has been reported among men who have sex with men - a group that includes curious, experimenting, bisexual and homosexual men, or SMBs for short.
Following reports of a large proportion of men from this group among all monkeypox cases, there are those who are trying to tag monkeypox as a “disease of the gay community”. Such labelling, which is based on misinformation and misunderstanding, could not only add an additional stigma to a group already suffering from discrimination, but also hinder efforts to protect the general population and prevent the disease from spreading.
However, ignoring the fact that the majority of patients belong to the same group could also make it difficult to contain the spread of monkeypox. This situation presents health authorities with a difficult challenge. They must act to reduce the risk of infection in the populations that are affected by the disease more than others, without causing prejudice or discrimination, while at the same time making it clear to the public that any person can contract the disease and that everyone should be careful.

The first outbreak out of Africa occurred in the US because of a shipment of rodents, including giant pouched rats and dormice, coming from Ghana. A dormouse, Graphiurus ocularis | Source: Handré Basson, Wikimedia Commons
About Monkeypox
The cause of the disease is the monkeypox virus. It belongs to the pox family of viruses (Poxviridae) and the genus Orthopoxvirus, which also includes the two viruses that caused smallpox and were eradicated thanks to a global vaccination effort. Despite the name similarity, the pox viruses are not related to the chickenpox disease, caused by a herpes virus.
Monkeypox so called because it was first discovered in monkeys, in two outbreaks that occurred in a research facility in Copenhagen, Denmark in 1958. Despite the name, it seems that the main hosts of the virus are actually rodents. The disease was first identified in humans in 1970, in a nine-month-old boy in the Democratic Republic of Congo, who was suspected of being infected with smallpox.
The virus was later discovered in other central and west African countries. Most of the patients live in the Democratic Republic of Congo. .The first outbreak outside of Africa – and the largest one up until the current outbreak – occurred in 2003 in the US, due to a shipment of rodents from Ghana, Africa to a pet store in Illinois, which included giant pouched rats and dormice. The imported rodents infected prairie dogs (large ground squirrels native to North America) which were housed next to them in the store and were later sold as pets. The pet owners were infected directly via bites and scratches, or indirectly following contact with excrements while cleaning the cages. Forty seven people were infected in this outbreak, but there were no fatalities and nor was there any human-to-human transmission of the disease.
The virus’s family tree includes two clades. The Central-African clade (originating from the Congo basin) is more contagious and more virulent, with a 10.6 percent fatality rate in infected individuals. The West-African clade has a fatality rate of 3.6 percent in patients diagnosed in Africa. The virus identified in the current outbreak outside of Africa is the one belonging to the West-African clade, which is significantly less deadly. It is likely that in Western countries, which have access to advanced medical care, fatality rates will be much lower, if not near zero.
Disease symptoms are similar to those of smallpox, but milder. They appear after an incubation period of five days to three weeks following infection, and, as far as we know, patients are not contagious at this stage. The first symptoms to appear are reminiscent of a cold. They usually include a fever and sometimes also a headache, muscle pain, back pain, sore throat, enlarged lymph nodes, chills and fatigue.
Between one and three days of the onset of symptom a rash appears, developing over time into fluid-filled (purpulent) blisters that eventually crust and fall off. The monkeypox rash is usually painful. It typically starts in the mouth (in the oral cavity) or on the tongue, spreads to the face and then to the limbs, and sometimes to the rest of the body. If the lesions reach the eyes, they may cause blindness. The disease usually lasts between two and four weeks, until all the survivors fully recover. As long as patients are symptomatic, they could be infectious.
In the current outbreak, the nature of the symptoms in many patients is slightly different, and can be manifested, for example, in a non-painful rash – sometimes a single lesion – in the genital area or anus, which appears without a fever and does not spread to other areas of the body. The Centers for Disease Control and Prevention (CDC) in the United States has even alerted doctors to be aware of that fact that not all patients have a fever, and that the rash can be local.
The CDC also emphasized that monkeypox is a possible diagnosis for any person, regardless of their travel history or sexual preferences. Such a diagnosis would be particularly likely in people who came in contact with patients, those who came back from abroad during the month preceding the onset of symptoms, and also especially in MSM who have genital lesions.
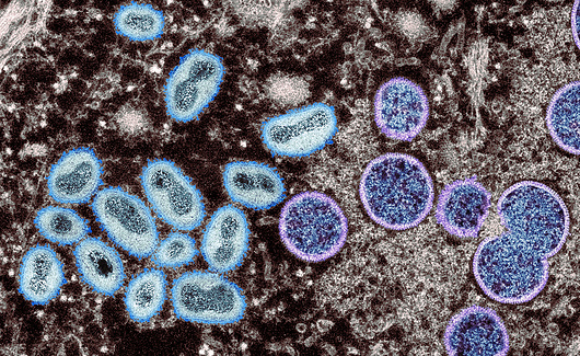
Can cause disease in humans and monkeys, but its main hosts are rodents. Monkeypox virus from a human skin sample | Source: CDC, Science Photo Library
An Everyman’s Disease or an MSM Disease?
Monkeypox can indeed infect anyone. The ongoing and worsening epidemic in Africa, and the outbreaks outside the continent, have shown beyond doubt that the virus has no boundaries. It can infect anyone, at any age, if they were in close contact with an infected animal, a human patient or with contaminated objects. During the current outbreak, the disease has already infected people of all kinds.
“While we see, for example, that some cases are among men who have sex with men, this is not a “gay disease”, as some people have tried to label it in social media”, said Andy Seale, a World Health Organization (WHO) advisor on HIV, hepatitis and sexually transmitted infections, during a Q&A session. “Anyone can contract monkeypox following close contact”.
The virus is transmitted through direct contact with saliva, or through exposure to large saliva droplets spread over a short distance. The virus can also be transmitted via direct contact with the rash, blood or fluids from blisters and scabs. Objects contaminated with the virus following patient contact, such as clothes, bedding, towels or foodware, may also become a source of infection. However, the widespread premise at the moment is that the virus does not easily transmit from person to person, and that normally, prolonged exposure is required in order to become infected with it.
If so, how did thousands of people get infected with the virus, and why are most of the infected young men who have sex with other men? The virus apparently had a bit of luck. In Europe, many restrictions set due to the COVID pandemic were lifted. Tourism has returned, and with it traveling from place to place, as have parties and mass events, in which many contacts occur between participants. This is a grand opportunity for the occurence of superspreading events of any infectious disease. The conditions were exactly right for the virus to spread.
Among the events that resumed were also some pride events, such as the Gay Pride events in Maspalomas on the Spanish Canary Islands, which were attended by tens of thousands of people from all over Europe, and which were connected to a number of monkeypox cases in the current outbreak. People from all over the world arrive to such events to rejoice and celebrate, and as adults from all genders and sexual orientations will confirm, many times, parties also involve sex.
Monkeypox is not considered a sexually transmitted disease. It’s true that the genetic material of the virus was recently discovered in semen of a number of patients, and it is even possible that it can contain infectious virus particles, but it is still not known whether one can become infected with the virus by coming in contact with semen. However, sexual intercourse involves close proximity, skin-to-skin contact and exposure to saliva, and usually for quite a while. These are optimal conditions for infection with the virus, and could explain its spread among sexually active young people, as well as the location of the rash.
Since monkeypox infection occurs upon close contact, which is not necessarily sexual, it would be reasonable to expect that the disease would spread mostly among members of communities who maintain close contact. Since infections started, by chance, in men at events of the LGBT community (but could have started just as easily at other parties and events), it is reasonable to expect that the disease will spread mainly among men within this community. According to the WHO and a number of researchers, another reason that more monkeypox cases are reported among MSM who contracted the disease following sexual activity, is that this population is more aware of diseases compared to the rest of the public and makes the effort to seek help at STD clinics and to get tested. Therefore, it could be possible that other people, who were infected in other ways, have not been tested and identified just yet.
However, at the current stage of theoutbreak, it is likely that if many people who are not men who have sex with men, were to be infected with monkeypox, these cases would already have been detected. Ashleigh Tuite, an epidemiologist from the University of Toronto, said to Science Magazine that she understands the concern of focusing on MSM, considering the risk of creating a stigma that could exacerbate discrimination against them. This was the case, for example, at the beginning of the COVID pandemic, which led to discriminatory and racist attitudes towards people of Asian descent.
“Stigma and blame undermine trust and capacity to respond effectively during outbreaks like this one”, said Matthew Kavanagh, Deputy Executive Director of the Joint United Nations Programme on HIV/AIDS (UNAIDS). “Experience shows that stigmatizing rhetoric can quickly disable evidence-based response by stoking cycles of fear, driving people away from health services, impeding efforts to identify cases, and encouraging ineffective, punitive measures”.
Since the disease is unrelated to sexual orientation or preference, and the virus can infect anyone, everyone should learn to identify the disease and know how to avoid it. When we recognize a disease in a specific group, we could actually be aiding its further transmission of it and endanger public health. For example, patients may not realize they’ve been infected, since they do not belong to the group with which disease is identified. Alternatively, they may deliberately avoid receiving treatment, so they are not mistaken for being members of the group, especially if there are negative stigmas associated with it.
However, according to Tuite, “based on the data that we have, and based on the contact tracing that’s been done, it’s very clear that this is an MSM-focused [monkeypox] outbreak at this point”.
“Anyone can get monkeypox, but we’re seeing disease activity primarily among MSM”, confirmed Demetre Daskalakis, an HIV prevention specialist at the CDC.
One of the reasons for this is that the virus has infected, within the community of men who have sex with men, a group of people who, relative to others, use to have sex more frequently, and with more partners. A report by the UK Health Security Agency, following interviews with 45 MSMs who contracted monkeypox due to their sexual habits, found that 44 percent of them reported on having more than ten sexual partners over the course of the past three months, and 44 percent reported that they participated in group sex during the incubation period of the disease. In addition, 30 percent reported that they were sexually active outside of their city of residence, 20 percent of these outside national borders and 24 percent reported having sex with men from abroad during the incubation period.
“It’s entirely possible for this epidemic to rage among a subset of people just because that subset is connected in a network differently than everyone else”, said Keletso Makofane, a social network epidemiologist from Harvard University. A research article recently published on the medRxiv website supports this claim (although it has not yet undergone meticulous peer review).
The research used data of the sexual habits of people from the UK to build models of monkeypox spread among men who have sex with men and in other groups. The models showed that infection of a sub-group of MSMs who have many sexual partners can explain the spread of monkeypox in the population. According to the models, if nothing is done to prevent this, the spread among men who have sex with men will be long and ongoing, with more than 10,000 new patients. However, an ongoing outbreak is not expected in other groups, and the number of new patients is expected to be anywhere between 10 and 10,000.
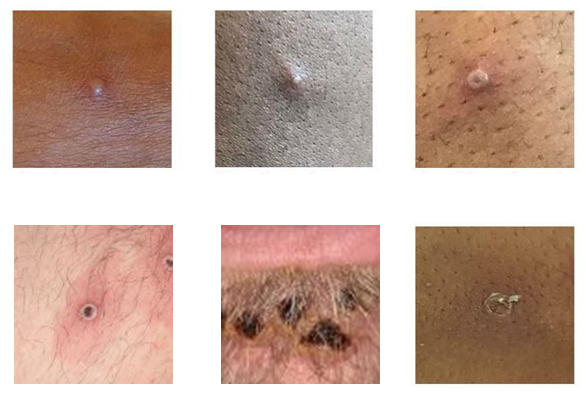
A rash that develops into fluid-filled blisters that eventually crust and fall off. Monkeypox lesions | Source: UK Health Security Agency
Risk Communication
In order to prevent this scenario, without causing a stigma that may interfere with the way we face monkeypox, and in order not to neglect the population in which the disease is most widespread, health authorities around the world, as well as organizations focusing on this subject, have launched a PR campaign targeted at the general population, including men who have sex with men.
The CDC, for example, published an ad explaining which intimate activities among sexually active people may transmit the virus: all types of sexual intercourse; hugs; massages and mutual masturbation; kisses and short distance conversations; and contact with fabric and objects a patient has touched – such as towels or sex toys. It also called on all people – regardless of their gender or sexual preferences – to visit their nearest clinic in any case that an unexplained rash or other symptoms appear; and, naturally, to avoid sexual contact or other intimate contact with people as long as lesions are present. At the same time, the CDC called on doctors to be suspicious of any rash disease similar to monkeypox, regardless of the patients’ characteristics or history. However, this suspicion does increase in cases when a rash appears in men who have reported having sexual contact with other men.
According to updates published by the UK Health Security Agency (UKHSA), although the risk to the public in the country is low, it is important for everyone to be alert to any new development of new rashes or of skin lesions. Since most known patients in the current outbreak are men who have sex with other men, the agency stressed that the members of this group need to be particularly aware of any symptoms, especially if they’ve recently had sex with a new partner. However, the agency's Chief Medical Advisor, Susan Hopkins, said that anyone suspected of having symptoms should avoid contact with others and seek medical care as soon as possible, especially if they’ve recently had a new sexual partner.
A report by the European Centre for Disease Prevention and Control (ECDC) states that infections in the current outbreak are likely related to multiple sexual partners, a behavior that is indeed characteristic of part of the MSM community. According to the report, the fact that most of the world today is no longer vaccinated against smallpox – a vaccine which is also effective against monkeypox – contributes to the spread of disease. The authors recommend that health authorities begin raising the awareness of the general public’s to monkeypox, issue instructions and guidelines on how to deal with it, and, at the same time, raise awareness among men who have sex with other men as to the outbreak that is occurring in this population group. The Center has indeed published ads directed at this group. It also issued temporary recommendations to health authorities regarding measures to help them prepare for upcoming summer events, including pride events.

Anyone can contract the disease, regardless of sexual orientation or preference, but participation in crowded events and close physical contacts increase the risk of infection. Pride event | Source: paparazzza, Shutterstoc.
What to do?
Anyone can become infected with monkeypox due to direct contact with a patient or, for example, due to contact with clothes or bedding used by him or her. If you present with symptoms – especially if you’ve been near a patient, recently returned from abroad, switched sexual partners, or are an MSM with multiple partners – see your doctor promptly to get checked. In addition, avoid having sex – a condom will not necessarily prevent a monkeypox infection – and avoid non-essential encounters with people.
Do not be shy and do not fear stigma. There are many ways to become infected with monkeypox, and there is no reason to assume someone was infected while having sex. And it of course does not have any bearing on their sexual orientation or preferences.
World experts currently don't recommend that people without symptoms change their behavior to avoid being infected, rather they recommend an “increased level of alertness”. We are still at the stage of the outbreak in which attention and alertness of the general public can prevent new infections and stop the spread of the disease. Providing information, along with the vaccination of caregivers, MSM with multiple partners, and of people who have been exposed to the virus, will make it possible to maintain everyone’s health, without fueling stigmas and spreading misleading and dividing information.
The article is based on a publication which first appeared in the blog “Noam’s arch – Biological thoughts”. The publication is courtesy of Noam Levitan and all rights are reserved to him.
