Learn about the different types of stroke, how they occur, the warning signs to look out for, and the available treatment options.
A stroke, also known as a cerebrovascular event, is a severe medical condition caused by a disruption of blood flow to the brain. This disruption leads to the death of nerve cells and other brain cells. The impaired cellular functions of the affected cells can lead to a decline in brain function, including speech and muscle control. Stoke is a life-threatening event, and it was the second leading cause of death worldwide in 2019, following heart attacks, as reported by the World Health Organization.
One of the primary factors that increases the risk of having a stroke is age, with the incidence of stroke events increasing significantly from the age of 55 and above. Other risk factors include high blood pressure, smoking which increases the likelihood of blockage of blood vessels, excessive alcohol consumption, which, among other things, can cause an increase in blood pressure, and cardiovascular diseases. There is also a negative correlation between socioeconomic status and the incidence of stroke and its impact. The lower an individual’s socioeconomic status, the higher the likelihood that they will experience a stroke, and the lower their ability to recover from it. This effect is attributed to disparities in access to quality healthcare services and the difficulty of maintaining a healthy lifestyle in lower socio-economic classes.
Types of Stoke
There are two main types of stroke: ischemic stroke and hemorrhagic stroke.
There are two main types of stroke: ischemic stroke and hemorrhagic stroke. Ischemic stroke is more prevalent, accounting for about 90% of all stroke cases. This condition occurs when an artery blockage in the brain restricts the supply of oxygenated blood to certain parts of the brain. This blockage can be caused by a blood clot or by a buildup of fatty deposits in the arteries that supply blood to the brain. When the blockage forms within a blood vessel in the brain itself, it is called a “thrombotic stroke”. In contrast, when the blocking factor forms elsewhere in the body and eventually becomes lodged in a narrow artery in the brain, it is called an “embolic stroke”.
An ischemic stroke that prevents blood supply only temporarily is called a “transient ischemic attack.” While such a stroke may not cause significant damage to the brain tissue, it should be treated as a serious warning sign. The occurrence of a transient ischemic attack signifies a high risk of a subsequent stroke; about one-third of individuals who experience a transient ischemic attack will also have a regular ischemic stroke within a year.
Hemorrhagic stroke is less prevalent than ischemic stroke and accounts for approximately 10% of all stroke cases. This condition occurs when one of the blood vessels in the brain ruptures, causing a significant amount of blood to leak into the brain tissue. This condition also compromises normal blood supply to certain cells, leading to their death.

Responsible for approximately 10% of stroke cases: Hemorrhagic Stroke. Image: GraphicsRF.com, Shutterstock.
The Warning Signs - How Can We Recognize a Stroke?
In case of a suspected stroke, it is crucial to bring the patient to the hospital immediately for prompt diagnosis and, if necessary, life-saving treatment. Early treatment is also essential to halt further damage to brain cells and to minimize the victim's functional impairment.
Since the stroke can damage various parts of the brain that fulfill different functions, the symptoms that arise can differ widely from person to person.The most common symptoms associated with a stroke are weakness or partial paralysis of the facial muscles on one side, which can cause a “crooked” smile or an inability to smile at all; weakness in the hands, to the extent of losing the ability to lift one or both hands; and difficulties in speech and comprehension.
Asymmetric weakness of facial or body muscles during a stroke occurs due to the fact that the control of the muscles on the right and the left side is performed separately by the brain’s two hemispheres. Typically, only one side is affected by the stroke, leading to loss of muscle control and thus weakness or paralysis only on one side of the body. Additional symptoms that may occur during a stroke include sudden blurred vision, memory loss, and confusion.

Signs of a stroke: weakness on one side of the face and hands, difficulty speaking, confusion, and more. artbesouro, Shutterstock
The Diagnosis
When a stroke is suspected, several tests are conducted at the hospital to diagnose the patient’s condition. In addition to general tests such as measuring of blood pressure, cholesterol, and blood sugar levels, a water-swallowing test is commonly performed. This is because impaired swallowing ability occurs in 30% to 78% of stroke cases.
If there is a genuine concern for stroke, it is customary to conduct brain scans to diagnose whether a blocked blood vessel is responsible for the stroke, find out which areas of the brain have been affected, and assess the extent of the damage. The two types of scans commonly used for this purpose are computed tomography (CT) and magnetic resonance imaging (MRI). CT scans are relatively faster and are often used for quick diagnosis of brain bleeding that requires urgent treatment. MRI scans are slower and more accurate than CT scans and are used when the symptoms are complex or when it is unclear where the stroke occurred, as well as after the occurrence of a transient ischemic attack. In both types of scans, doctors can inject a special substance into the patient’s bloodstream to improve the quality of the imaging and allow for a more thorough examination of the blood vessels in the brain.
Additional tests may be performed after a stroke to identify its source. For example, an ultrasound test allows doctors to check for narrowing or blockages in the blood vessels in the neck that supply blood to the brain.
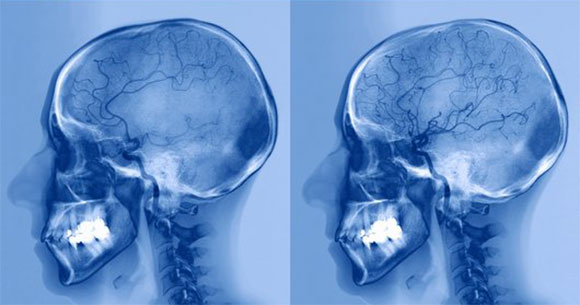
A before-and-after comparison of brain imaging showing a stroke patient with an artery blockage (left) and the same patient following treatment (right) with drugs that dissolve blood clots to alleviate the blockage. Source: ZEPHYR, Science Photo Library.
Treatment and Prevention
There are immediate treatments that can alleviate the patient’s condition and deal with the stroke before it worsens. Accurately diagnosing the type of stroke is of utmost importance because each type requires different treatment.
When dealing with ischemic stroke, the standard procedure involves administering drug therapy to dissolve blood clots, open the blockage formed in the brain’s blood vessels, and prevent the formation of new blood clots. Anticoagulants, also known as “blood thinners”, can increase the risk of bleeding and should not be used on patients with hemorrhagic stroke as they may exacerbate the situation.
A more invasive treatment involves catheterizing the blood vessels in order to dissolve or remove the blockage. A brain catheterization completed within two hours of the injury can significantly improve the chances and speed of recovery.
To treat a hemorrhagic stroke, it is customary to use medications to lower blood pressure, reduce the bleeding, and allow the rupture in the damaged blood vessel to heal. In some cases, it is possible to perform surgery in order to stop local bleeding. Such surgical options may include removing the problematic blood vessel in the brain, using a thin mesh to block the leaking blood, or "pinching" the leaking part of the blood vessel to prevent further bleeding.
Additionally, to lower the risk of stroke recurrence, the patient should make lifestyle adjustments based on their specific stroke risk factors. For example, if the stroke is believed to be caused by elevated cholesterol levels in the bloodstream, adopting a low-cholesterol diet and taking medications that reduce cholesterol levels are strongly recommended.
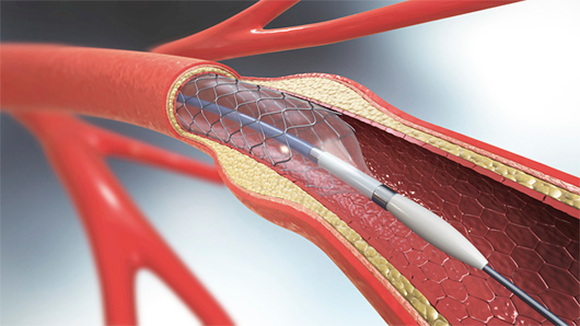
Brain catheterization completed within two hours of the initial injury significantly increases the chances of recovery. Illustration of arterial catheterization in the brain. Source: Christoph Burgstedt, Science Photo Library.
Post-Stroke Recovery
Addressing the patient’s rehabilitation and improving their functionality and quality of life is crucial after a stroke. Since the brain’s capacity to recover from the damage caused by stroke is often limited, long-term impairment in areas such as speech, walking, muscle control and cognitive clarity may persist. Coping can be improved through various means, such as therapy, physiotherapy, and occupational therapy. Ongoing research in this field aims to identify the most effective techniques for maximizing patient recovery, including electrical stimulation, gait exercises, Tai Chi, and more. As healthcare providers continue to gather knowledge, they are better equipped to offer meaningful treatments that can be implemented over an extended period of time, to achieve lasting progress.
Stem cell treatment is another promising new field that has the potential to improve the condition of stroke victims. Stem cells are undifferentiated cells whose final function has not yet been determined. They have the ability to differentiate into various cell types, making it possible to use them to rebuild parts of the brain tissue that were damaged by the stroke. While studies regarding this treatment are currently performed mainly in mice, it is possible that stem cells will be used to treat stroke in humans in the future.
Stroke is a life-threatening condition and there is much to learn about how to manage it and its consequences. Maintaining a healthy lifestyle that includes regular physical activity and a balanced Mediterranean diet can reduce the risk of having a stroke. Being aware of the typical symptoms of stroke is crucial, as it enables us to seek immediate medical attention for victims and prevent unnecessary damage.
